Summary Card
Overview
Upper eyelid ptosis is the abnormal drooping of the upper eyelid due to dysfunction of the levator palpebrae superioris or Müller’s muscle — distinct from pseudoptosis caused by extraocular factors.
Aetiology
Ptosis can be either congenital, due to levator dysgenesis, or acquired, which is further classified as myogenic, traumatic, neurogenic, or mechanical.
Diagnosis
Upper eyelid ptosis assessment involves a detailed history, examination, and specialist tests. The aim is to determine aetiology, degree of ptosis, and levator function. These factors influence surgical management.
Treatment
Surgical management is dependent on the surgeon’s preference, degree of ptosis, and levator function. Options include skin resection, muscle shortening, fat resection, and aponeurosis repair.
Updated by: Benedetta Agnelli, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Upper Eyelid Ptosis
Upper eyelid ptosis is the abnormal drooping of the upper eyelid due to dysfunction of the levator palpebrae superioris or Müller’s muscle — distinct from pseudoptosis caused by extraocular factors.
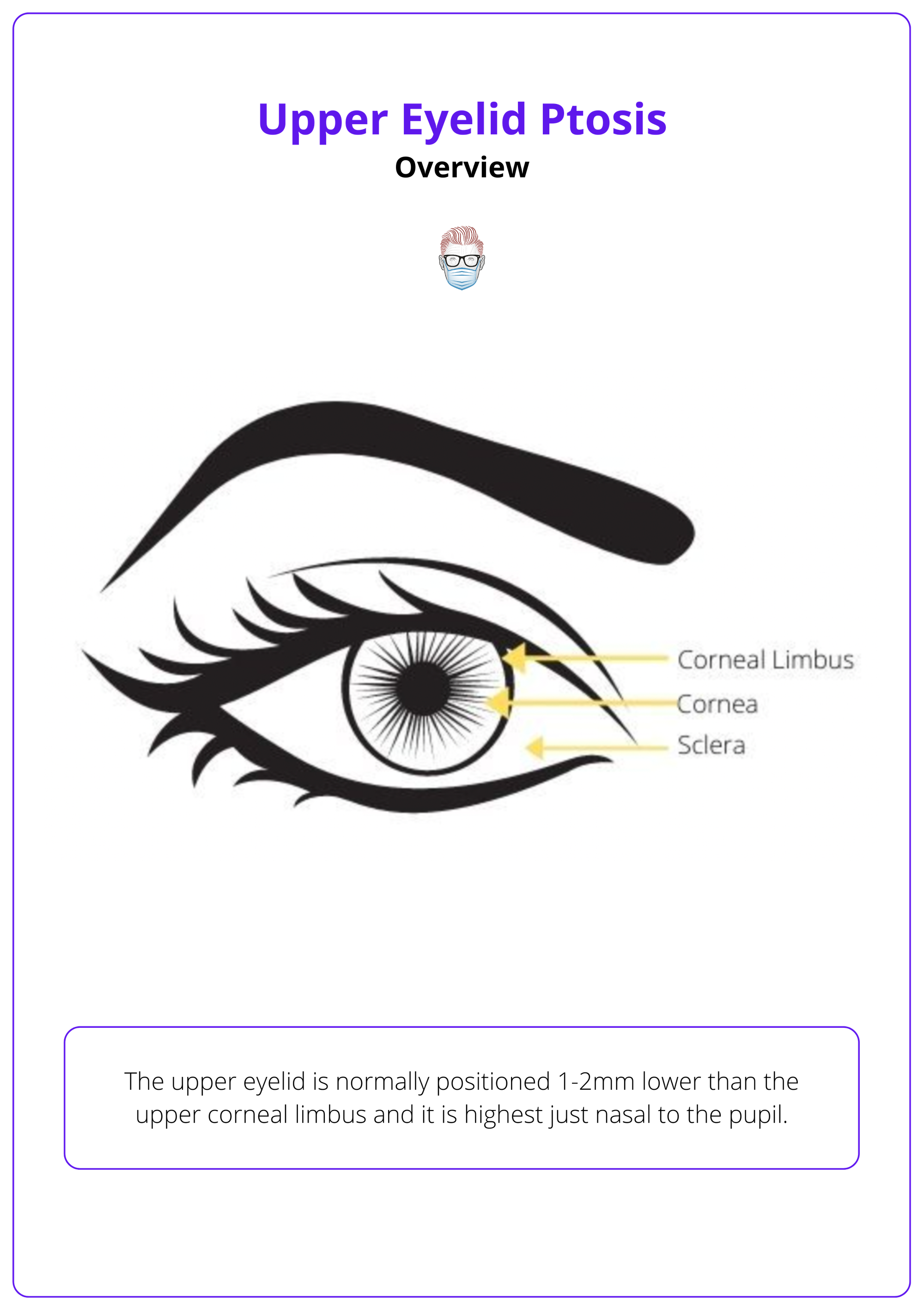
Upper eyelid ptosis, also known as Blepharoptosis is defined as an abnormal low-lying upper eyelid margin with the eye in primary gaze. The upper eyelid is normally positioned 1-2mm lower than the upper corneal limbus and it is highest just nasal to the pupil.
Ptosis is the result of the dysfunction of one or both upper eyelid elevator muscles.
- Levator Palpebrae Superioris Muscle: The primary elevator. Striated muscle, innervated by oculomotor nerve (CN III)
- Müller's Muscle: Simpathetically innervated smooth muscle.
The image below illustrates the upper eyelid.
Differentiate True ptosis from Pseudoptosis! Pseudoptosis is apparent ptosis not caused by an issue related to eyelid elevation, but for example from brow ptosis, enophtalmos, etc. (McCord, 1988).
Aetiology of Upper Eyelid Ptosis
Ptosis can be either congenital, due to levator dysgenesis, or acquired, which is further classified as myogenic, traumatic, neurogenic, or mechanical.
Understanding ptosis aetiology is critical for accurate diagnosis and appropriate management, as causes range from developmental defects to neuromuscular disorders or mechanical obstructions.
Acquired Eyelid Ptosis
Acquired ptosis arises later in life and is categorized into myogenic, traumatic, neurogenic, or mechanical origins.
- Myogenic: Includes involutional myopathic (senile) ptosis, the most common type, caused by levator aponeurosis laxity with preserved dermal attachments (raised supratarsal crease), and chronic progressive external ophthalmoplegia, a muscular dystrophy affecting extraocular muscles and the levator.
- Traumatic: Second most common type. Different causes can occur after cataract surgery, from dehiscence of the levator aponeurosis.
- Neurogenic: Includes third nerve palsy (levator paralysis), Horner’s syndrome (Müller’s muscle paralysis), and myasthenia gravis, where ptosis worsens with fatigue and improves with neostigmine or edrophonium.
- Mechanical: Caused by factors like upper lid tumors, severe dermatochalasis, or scarring that physically restricts eyelid elevation.
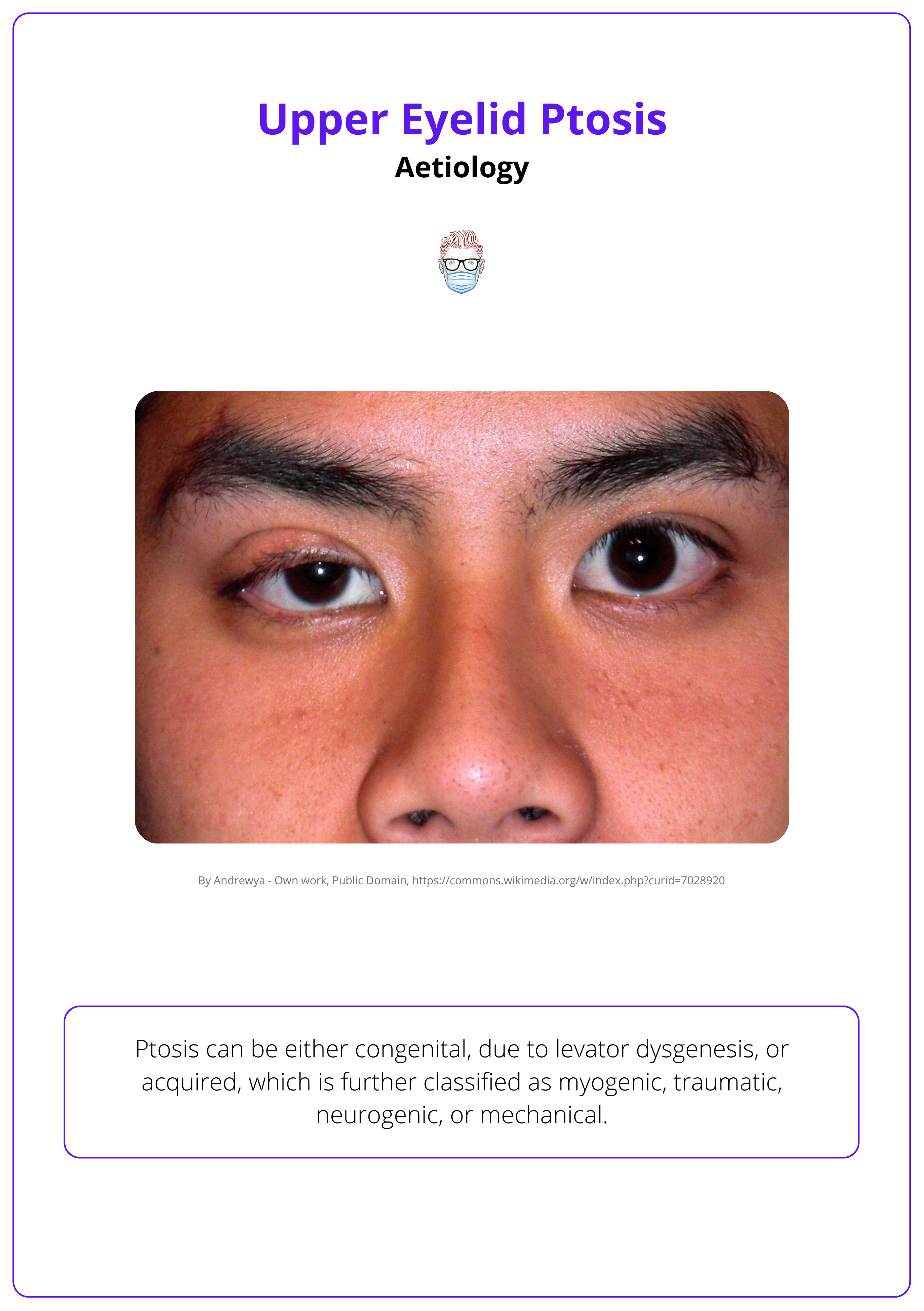
The image below illustrates mild right-eyelid ptosis.
Neurogenic ptosis in Horner's syndrome is easily identified as it improves with sympathomimetic agents (e.g. phenylephrine hydrochloride).
Congenital Eyelid Ptosis
Congenital ptosis is present at birth and stems from developmental anomalies in eyelid musculature.
- Levator Dysgenesis: The levator muscle is underdeveloped and often replaced by fibrous tissue, leading to minimal or absent eyelid elevation.
- Absent Supratarsal Crease: A hallmark sign due to poor levator function.
- Non-Progressive: Typically stable after birth and identifiable early in life.
Congenital ptosis presents at birth with lagophthalmos on downgaze (levator fibrosis), while acquired ptosis appears later without this feature.
Diagnosis of Upper Eyelid Ptosis
Requires history, eyelid measurements, and key functional tests (levator function, Bell’s phenomenon, pupil exam) to identify the cause and guide treatment.
A structured approach is essential to distinguish congenital from acquired ptosis, focusing on eyelid position, excursion, neuromuscular function, and compensatory signs. The following video by Ric Caesar is a detailed assessment of ptosis.
The examinations of ptosis is guided by the MEASUREMENT & LEVATOR SEVERITY mnemonic.
- M: Myosis/Mydriasis
- Differentiate Horner’s from Third Nerve Palsy.
- Anisocoria that is more noticeable in darkness suggests Horner’s syndrome, while prominence in light points to third cranial nerve palsy.
- E: Eyelid Closure
- Check for lagophthalmos and Bell’s phenomenon.
- Lagophthalmos, especially in congenital cases, raises risk of corneal exposure. A poor Bell’s reflex heightens postoperative keratitis risk.
- A: Abnormalities in External Eyelid Examination
- Rule out pseudoptosis causes.
- Brow ptosis, dermatochalasis, or enophthalmos can mimic true ptosis and must be excluded.
- S: Skin Crease
- Evaluate the supratarsal fold.
- Congenital ptosis often lacks a crease. Normal margin-crease distances are 6–8 mm in men and 9–11 mm in women.
- U: Unilateral or Bilateral
- Note the laterality of ptosis.
- Important for distinguishing between localized and systemic causes.
- R: Corneal Reflex
- Check for reduced corneal sensation.
- Important to identify pre-existing risk factors for ocular surface disease post-surgery.
- E: Errors in Vision and Refraction
- Perform baseline visual field testing.
- Essential for documenting functional impact and monitoring outcomes.
- M: Myasthenia
- Test for fatiguability and related signs.
- Use the ice test, Cogan’s lid twitch, or edrophonium trial for confirmation.
- E: Evaluation of History
- Clarify onset and progression.
- Helps distinguish between congenital and acquired forms.
- N: Neural Coordination (Hering’s Law)
- Observe for contralateral eyelid droop on lifting ptotic lid.
- A sign of equal innervation to both levators; correcting one side may unmask the other (Parsa 2001).
- T: Tear Film
- Assess dry eye status.
- Tear film insufficiency can exacerbate exposure risks post-correction.
- Levator Function
- Assessed using Burke’s method by measuring the eyelid excursion from downgaze to upgaze while manually immobilizing the frontalis muscle to prevent compensation.
- Severity
- Ptosis severity is classified as mild (1-2 mm), moderate (3 mm), or severe (≥4 mm), measured as the difference in upper eyelid position compared to the contralateral eye.
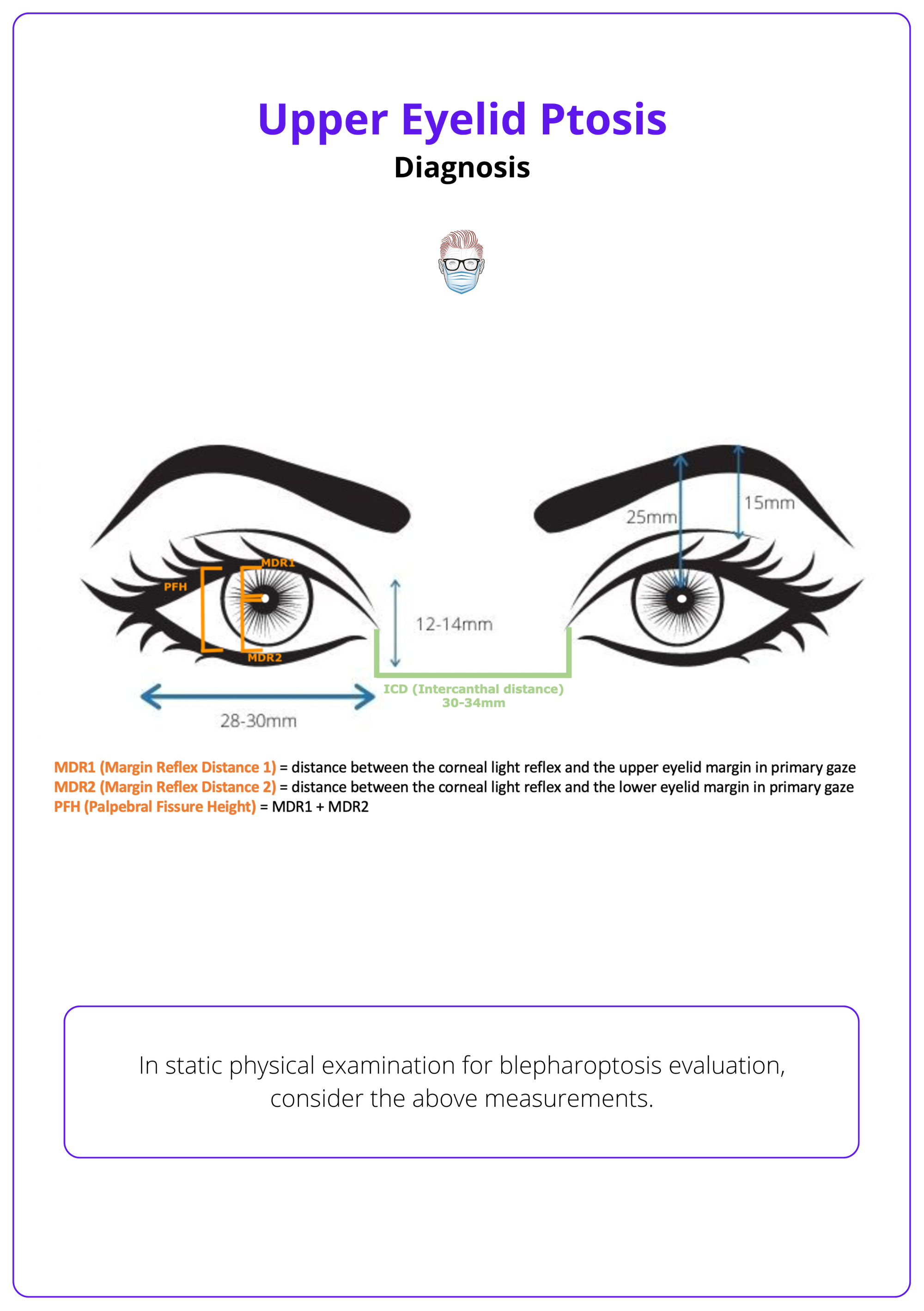
Eyelid measurements are summarised in the image below.
Like Hering’s phenomenon, the "Curtain Sign" in myasthenia gravis occurs when lifting the ptotic eyelid causes the contralateral eyelid to drop, likely due to an imbalance in neuromuscular compensation.
Treatment of Upper Eyelid Ptosis
Surgical treatment of ptosis is tailored to the degree of eyelid droop and the strength of the levator muscle, with procedures ranging from aponeurosis repair to frontalis suspension.
Managing upper eyelid ptosis requires matching the surgical technique to the functional anatomy of the eyelid, particularly levator muscle performance. Patient-specific factors, such as severity of ptosis and surgeon expertise, guide the selection of procedures aimed at restoring both function and aesthetics.
Müller’s Muscle-Conjunctival Resection (Fasanella-Servat Procedure)
- Minimally invasive option for mild ptosis.
- Involves resection of Müller’s muscle and conjunctiva without an external incision.
- Indicated in patients with good levator function and a positive phenylephrine test.
Levator Aponeurosis Repair
- Addresses aponeurotic dehiscence in moderate ptosis.
- Tightens or reattaches the levator aponeurosis to the tarsal plate.
- Anterior Approach: Via skin incision, allows direct visualization and adjustment.
- Posterior Approach: Through the conjunctiva, preferred in milder cases.
Here is a video by Ric Caesar demonstrating a type of posterior approach.
Posterior Approach for Ptosis Correction
Levator Resection or Advancement
- Shortens or repositions the levator complex.
- Suitable for moderate to severe ptosis with some levator function.
- Anterior Approach: Offers broader exposure for major adjustments.
- Posterior Approach: Less invasive; relies on residual Müller’s function.
Frontalis Suspension (Crawford or Fox Technique)
- For severe ptosis with poor or absent levator function.
- Connects the eyelid to the frontalis muscle using sling material, enabling eyelid lift via brow elevation.
- Crawford Technique: Uses a looped sling for better contour.
- Fox Technique: Uses a straight sling configuration.
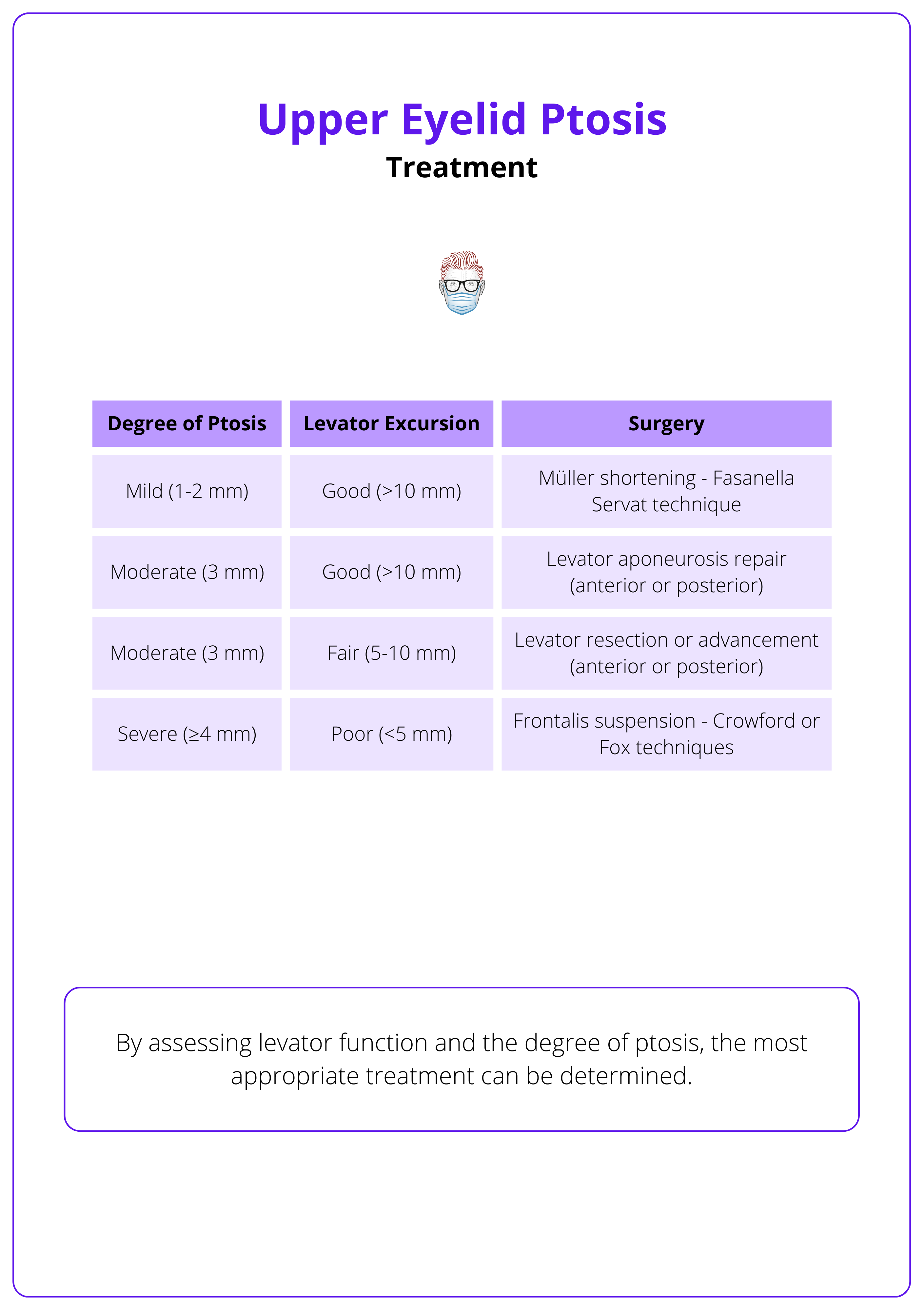
The image below summarizes upper eyelid ptosis treatment options.
Botox-induced ptosis can occur if the toxin diffuses to the levator muscle, temporarily weakening it. Sympathomimetic eye drops (e.g., apraclonidine) may help lift the eyelid until Botox effects subside.
Conclusion
1. Overview: Understanding the condition of upper eyelid ptosis and differentiating it from pseudoptosis.
2. Aetiology & Classification: Understanding the various causes of ptosis and its classification by etiology is essential for accurate diagnosis. Learning how to differentiate between types of ptosis and perform a thorough differential diagnosis.
3. Diagnosis: Identifying the key parameters that must be assessed to ensure an accurate ptosis evaluation and guide the appropriate treatment. To simplify this process, we provide a mnemonic to help remember the essential steps.
4. Treatment: Familiarizing with proper classification of ptosis and assessment of levator function is crucial for selecting the most appropriate surgical technique. Learning the key characteristics of different procedures to guide optimal treatment for each patient.
Further Reading
- Finsterer J. Ptosis: causes, presentation, and management. Aesthetic Plast Surg. 2003 May-Jun;27(3):193-204. doi: 10.1007/s00266-003-0127-5. Epub 2003 Aug 21. PMID: 12925861.
- Wong CH, Hsieh MKH, Mendelson B. Upper Eyelid Ptosis Correction with Levator Advancement Using the Levator Musculoaponeurotic Junction Formula in White Patients. Plast Reconstr Surg. 2024 Jun 1;153(6):1403-1414. doi: 10.1097/PRS.0000000000010889. Epub 2023 Jun 27. PMID: 37387609; PMCID: PMC11104497.
- Frueh BR. The mechanistic classification of ptosis. Ophthalmology. 1980 Oct;87(10):1019-21. doi: 10.1016/s0161-6420(80)35135-x. PMID: 7017524.
- Jelks GW, Jelks EB. The influence of orbital and eyelid anatomy on the palpebral aperture. Clin Plast Surg. 1991 Jan;18(1):183-95. PMID: 2015744.
- Jelks GW, Jelks EB. Preoperative evaluation of the blepharoplasty patient. Bypassing the pitfalls. Clin Plast Surg. 1993 Apr;20(2):213-23; discussion 224. PMID: 8485931.
- Bartlett SP, Wornom I 3rd, Whitaker LA. Evaluation of facial skeletal aesthetics and surgical planning. Clin Plast Surg. 1991 Jan;18(1):1-9. PMID: 2015737.
- Farkas LG, Kolar JC. Anthropometrics and art in the aesthetics of women's faces. Clin Plast Surg. 1987 Oct;14(4):599-616. PMID: 3652607.
- McCord CD Jr. The evaluation and management of the patient with ptosis. Clin Plast Surg. 1988 Apr;15(2):169-84. PMID: 3280214.
- Parsa FD, Wolff DR, Parsa NN, Elahi aE E. Upper eyelid ptosis repair after cataract extraction and the importance of Hering's test. Plast Reconstr Surg. 2001 Nov;108(6):1527-36; discussion 1537-8. doi: 10.1097/00006534-200111000-00014. PMID: 11711923.
- Chang S, Lehrman C, Itani K, Rohrich RJ. A systematic review of comparison of upper eyelid involutional ptosis repair techniques: efficacy and complication rates. Plast Reconstr Surg. 2012 Jan;129(1):149-157. doi: 10.1097/PRS.0b013e318230a1c7. Erratum in: Plast Reconstr Surg. 2015 May;135(5):1507. PMID: 22186506.


