Summary Card
Introduction
Breast augmentation addresses cosmetic and reconstructive needs, with contraindications including unrealistic expectations, body dysmorphia, infections, cancer, and pregnancy/lactation.
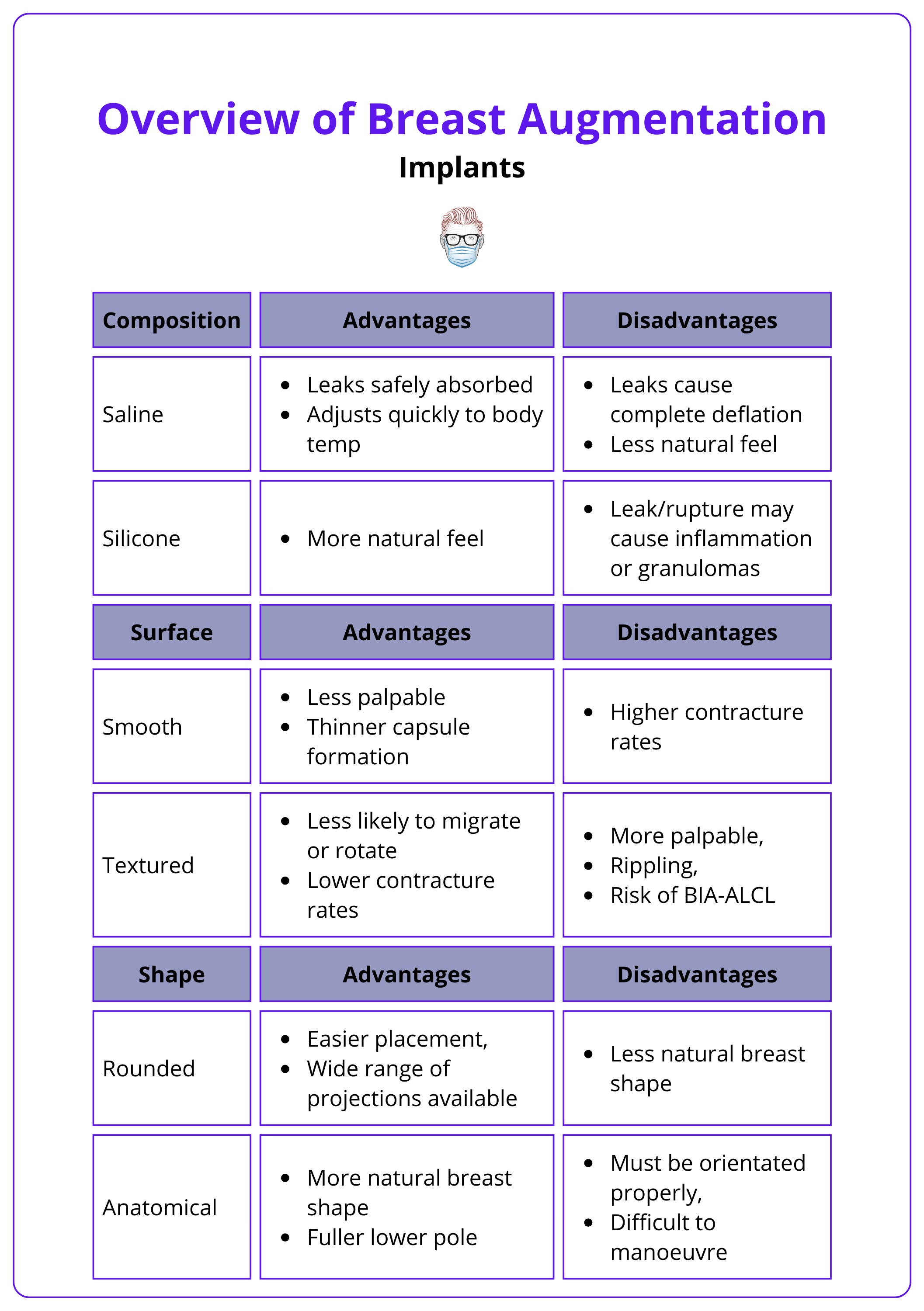
Implants
Implants vary by composition (silicone vs. saline), surface (smooth vs. textured), and shape (round vs. anatomical), and implant selection can be based on patient desires, anatomy, and surgeon experience.
Clinical Assessment
A thorough aesthetic consultation for breast augmentation includes a detailed history, comprehensive breast examination, photographic documentation, and breast metrics.
Surgical Incisions
Breast augmentation involves selecting an incision at an inframammary, periareolar, or transaxillary site.
Surgical Planes
Implant pocket planes include subglandular, subfascial, subpectoral, or dual plane.
Complications
Complications of breast augmentation, though rare, can include infection, hematoma, seroma, changes in nipple sensation, capsular contracture, implant leakage or rupture, asymmetry, implant migration, BIA-ALCL, and interference with breast cancer screening.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Waruguru Wanjau, Educational Fellow.
Introduction to Breast Augmentation
Breast augmentation is the surgical increase in breast volume, commonly with the use of implants, for cosmetic or reconstructive purposes.
Breast augmentation, also known as augmentation mammoplasty, is defined as the surgical increase in breast volume.
Indications
The main indications for breast augmentation surgery are:
- Cosmetic enhancement
- Post-pregnancy volume loss
- Asymmetry correction
- Reconstructive purposes
- Congenital anomalies (eg: tuberous breast deformity, Poland syndrome)
Contraindications
Certain conditions and factors contraindicate breast augmentation:
- Unrealistic expectations
- Body dysmorphia
- Active infections
- Breast cancer: untreated or active breast malignancy, ongoing oncological treatment
- Pregnancy and lactation
The most common form of breast augmentation is in the form of non-autologous breast implants. However, autologous fat transfer is another option where lower volumes of augmentation are desired. A combination of implant-based augmentation with lipofilling to mask implant edges has also been described (Adams, 2012)
Implants for Breast Augmentation
Silicone implants are the most commonly used worldwide, with their shape and surface attributes contributing to implant choice based on individual needs.
Implants differ in their composition, surface characteristics, and shape, being utilised in different circumstances to achieve the desired result.
- Composition: silicone implants vs saline implants
- Surface: textured vs. smooth
- Shape: round vs. anatomical
The characteristics of implants with the advantages and disadvantages guiding implant choice are summarised in the table below (Coombs, 2019).
Selecting the right implant involves considering several factors.
- Patient's preference: The desired size, shape, and projection.
- Patient's anatomy: Breast analysis and accurate measurements.
- Surgeon's experience: Surgeon's familiarity with different types of implants (Adams, 2016).
- Cost: Payers (patient or health system’s) ability to afford the specific implant.
Clinical Assessment for Breast Augmentation
A detailed history, physical examination, and breast metrics are vital for decision-making in breast augmentation surgery.
An aesthetic consultation should be thorough, gathering all the useful information to aid in implant choice and surgical approach.
History
- Personal and familial history of breast disease and malignancy
- Pregnancy history and family planning
- Current and desired breast size
- Up to date with cancer screening protocols
Examination
- Breast examination of all 4 quadrants and axillary tail - looking for masses, dimpling, NAC changes, or discharge
- Skin quality
- Chest wall and breast symmetry noting any changes in size, IMF, and NAC height.
- Breast footprint – vertical and horizontal dimensions
- BMI
Breast Measurements
- Sternal notch to nipple distance (SN-N)
- Nipple to IMF distance (N-IMF)
- Breast base width
- Parenchymal coverage (pinch test)
- Anterior pull skin stretch - length of the stretch from resting to maximal projection with pull at the edge of the areola
- Parenchymal fill - the percentage of skin envelope filled by parenchyma (Xi, 2014)
Consider imaging (such as mammogram ± ultrasound), if not already performed as part of screening.
The ‘High-Five System’ is an objective algorithm for determining breast implant size based on standardised measurements and has reported excellent results and low complication rates. (Tebbetts, 2006).
Surgical Incisions for Breast Augmentation
There are various incision sites for breast augmentations. These include, but are not limited to inframammary, periareolar, or transaxillary.
The surgical technique for breast augmentation requires selecting a suitable incision site and determining the optimal pocket plane for implant placement. Popular incision placements include:
Inframammary fold incision
- Well hidden scar
- Allows great access and control of pocket dissection
Periareolar Incision
- Well hidden scar
- Unlikely to cause sensory disturbance of the nipple compared to the inframammary technique
- Contamination theory – ductal commensals more likely to cause biofilm and contracture
The image below illustrates surgical incisions for breast augmentation.
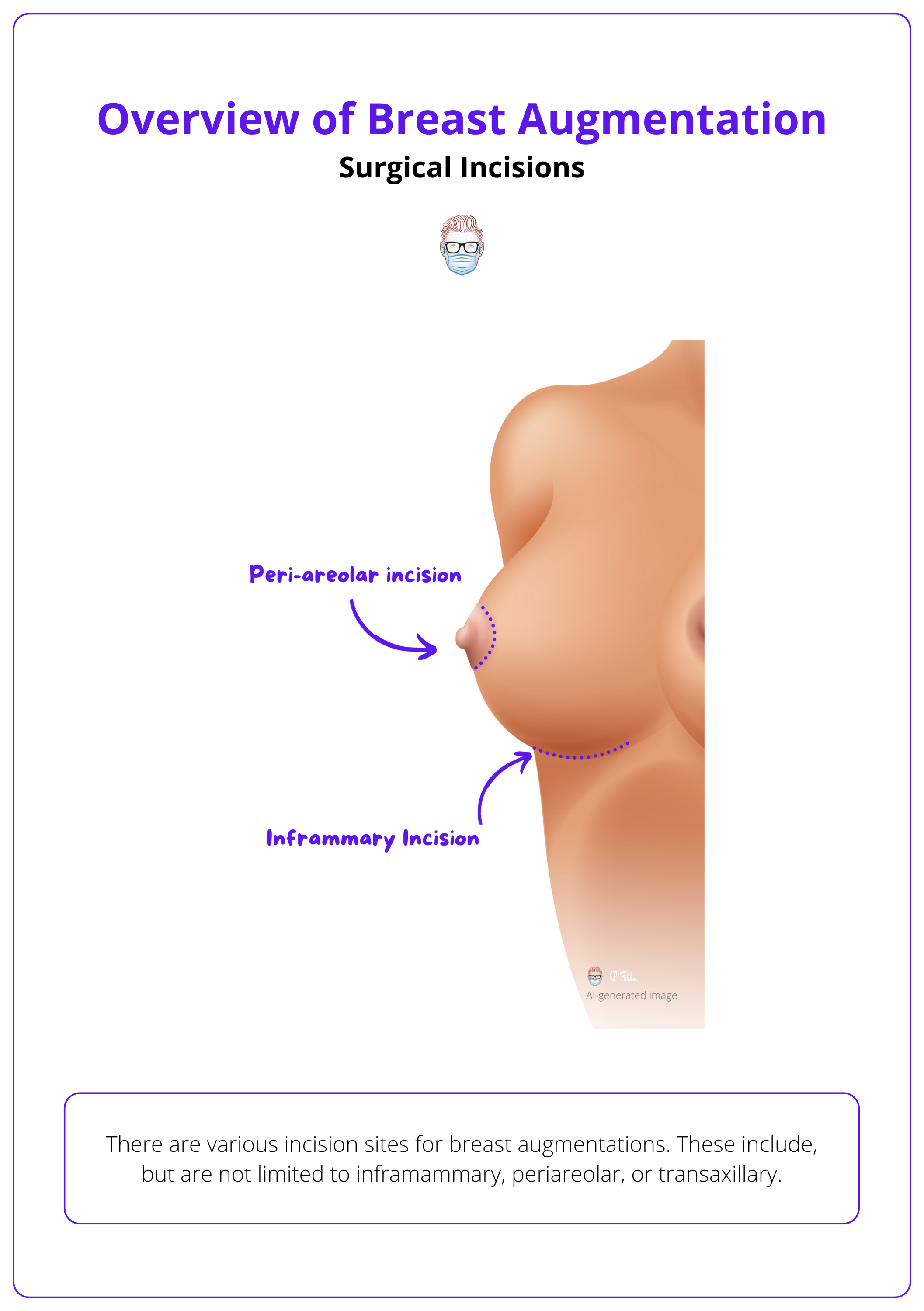
The transaxillary incision is less commonly used. The benefit is that there is no scar on the breast. It is limited, however, by a difficult dissection and implant insertion.
A transumbilical approach also exists but is not widely used as it involves blind dissection is limited to using saline implants, and is associated with less satisfactory outcomes.
Surgical Planes for Breast Augmentation
A breast implant can be inserted/placed into the subglandular, subpectoral, subfascial, or dual plane.
Pocket dissection and choosing the right plane for implant placement depend upon implant characteristics, surgeon preference, patient anatomy, and lifestyle. The implants can be inserted into a single plane or dual plane.
Single Plane
The most commonly used single pockets/plans are listed below.
- Subglandular: Dissection and pocket development are deep to the breast gland but superficial to the pectoralis major muscle and fascia.
- Subfascial dissection, lifting the pectoralis fascia but superficial to the pectoralis major.
- Subpectoral: Dissection is deep to the pectoralis major muscle but superficial to the pectoralis minor.
The image below illustrates the implant pocket for breast augmentation.
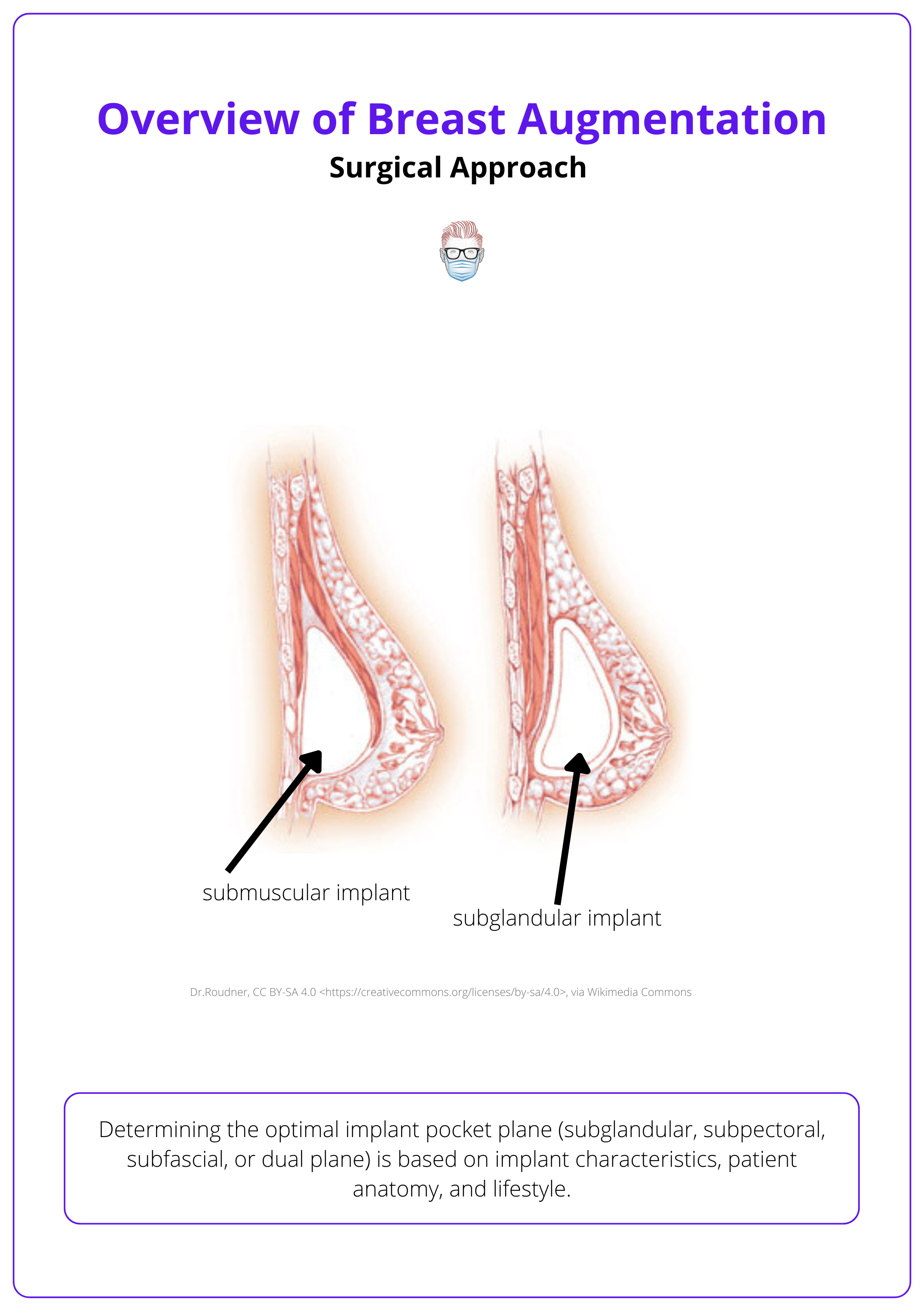
Dual Plane
Dissection in both planes with the upper portion of the implant being covered by pectoralis major and the lower portion being subglandular. The extent of subglandular dissection depends on the degree of ptosis.
3 types of dual-plane approaches are described, depending on the extent of dissection:
- Type 1 involves releasing the muscle at IMF and is used when no ptosis exists.
- Type 2 involves releasing the muscle at IMF and subglandular dissection up to the lower border of NAC.
- Type 3 is similar to type 2 but subglandular dissection is taken up to the superior border of NAC.
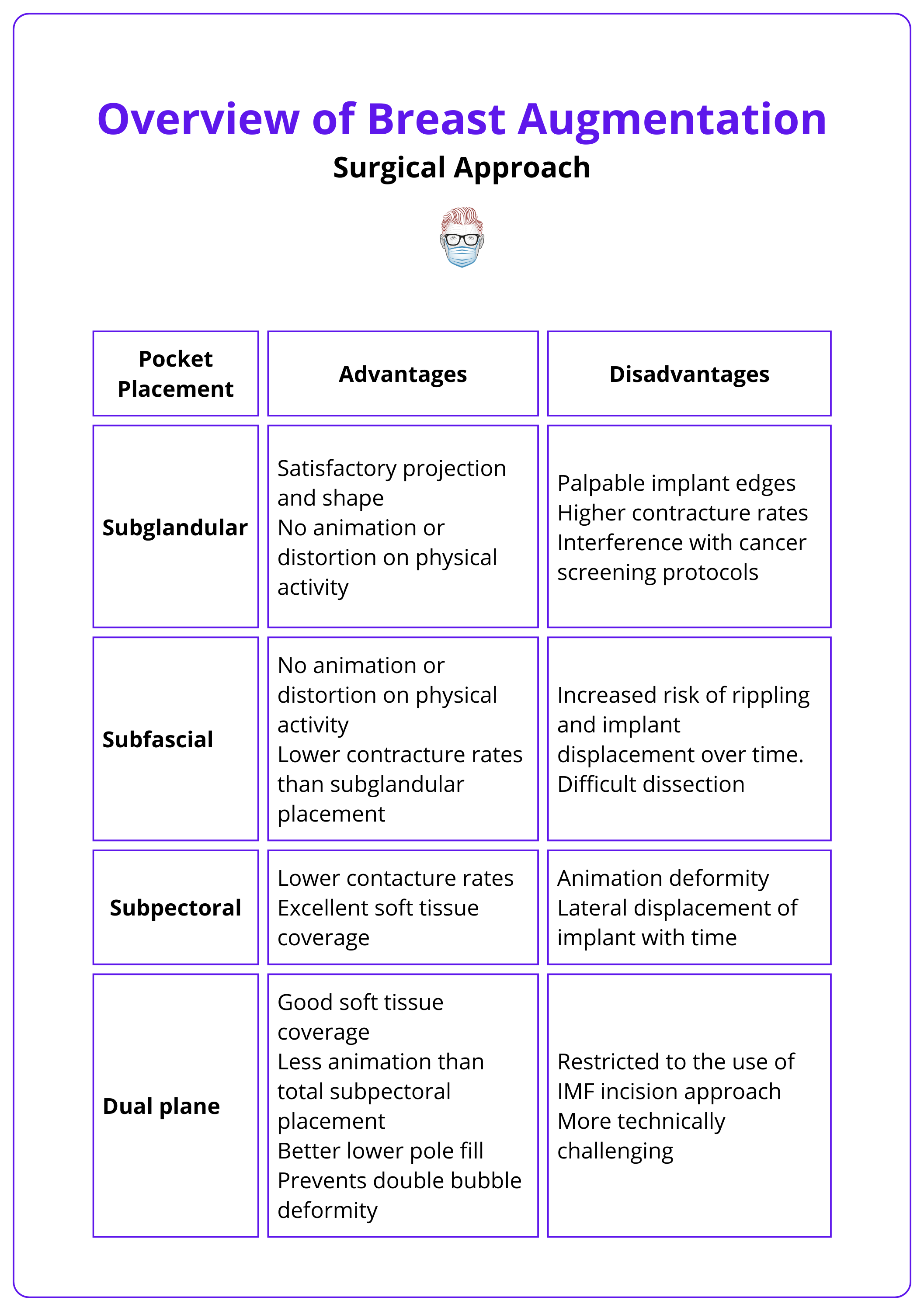
Comparison of Implant Location
The advantages and disadvantages of each pocket plane are summarised in the table below (Stutman, 2012):
Complications of Breast Augmentation
Similar to any cosmetic procedure, complications may be implant-related, requiring revision surgery, or more serious complications such as BIA-ALCL.
General Complications
Complications are rare but can lead to unsatisfactory aesthetic results and potential medical morbidity (Bengtson, 2009). These can relate to soft tissue and implant issues. More specifically:
- Cosmetic: Asymmetry, scar hypertrophy/keloid.
- Soft Tissue: infection, wound dehiscence, haematoma and seroma, changes in nipple sensation.
- Implant: infection, leakage or rupture, implant rotation, double bubble deformity.
Specific Complications
Capsular Contracture
This was classified by Baker into 4 grades depending upon the palpability and visibility of an implant (Baker, 1995).
- Grade I: Breast is soft and appears natural.
- Grade II: Breast is firm with implant palpable but not visible.
- Grade III: Breast is firm, with implant palpable and visible.
- Grade IV: Breast is hard, painful, and distorted.
Breast Implant-ALCL (BIA-ALCL)
This is a rare type of T-cell lymphoma that develops in the scar tissue and fluid surrounding breast implants, predominantly associated with textured implants.
It typically presents as a late-onset seroma or palpable mass and requires prompt treatment with en bloc capsulectomy and implant removal.
It is recommended that all late-onset seromas should be aspirated under ultrasound guidance, with mandatory cytology and CD30+ immunohistochemistry to rule out BIA-ALCL (di Pompeo, 2018).
It also interferes with cancer screening, specifically subglandular implants
To ensure accurate screening protocols, patients with subglandular implants should get an Eklund view in mammography apart from the standard views (Sa dos Reis, 2020).
Breast Implant Illness
This is an emerging clinical condition with inflammatory and autoimmune symptoms. It is yet to be universally recognized as an accepted clinical entity.
Common presenting symptoms include fatigue, anxiety, chronic pain, and endocrine, autonomic, and peripheral nervous system dysfunction. It currently has no standard of care or guideline, but the majority of affected patients have a bilateral implant explantation with an aim to relieve symptoms. (Serena, 2023)
Conclusion
1. Understanding of Breast Augmentation: Gained insights into the surgical enhancement of breast volume, including cosmetic and reconstructive uses.
2. Clinical Assessment: Understood the necessity of detailed pre-surgical consultations including history, physical examination, and measurements.
3. Surgical Techniques: Learned about different surgical approaches and the importance of implant pocket placement.
4. Complications: Recognized potential complications like infection, capsular contracture, and implant issues such as rupture.
Further Reading
- Adams, William P. Jr. M.D.; Mallucci, Patrick M.D. Breast Augmentation. Plastic and Reconstructive Surgery 130(4):p 597e-611e, October 2012. | DOI: 10.1097/PRS.0b013e318262f607
- Coombs, Demetrius M., et al. "Breast augmentation surgery: Clinical considerations." Cleve Clin J Med 86.2 (2019): 111-122.
- Adams, William P. Jr. M.D.; Mckee, Daniel M.D. Matching the Implant to the Breast: A Systematic Review of Implant Size Selection Systems for Breast Augmentation. Plastic and Reconstructive Surgery 138(5):p 987-994, November 2016. | DOI: 10.1097/PRS.0000000000002623
- Xi, W., Perdanasari, A.T., Ong, Y. et al. Objective Breast Volume, Shape and Surface Area Assessment: A Systematic Review of Breast Measurement https://doi.org/10.1007/s00266-014-0412-5
- Tebbetts, John B., and William P. Adams. "Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process." Plastic and reconstructive surgery 116.7 (2005).
- Stutman, R.L., Codner, M., Mahoney, A. et al. Comparison of Breast Augmentation Incisions and Common Complications. Aesth Plast Surg 36, 1096–1104 (2012). https://doi.org/10.1007/s00266-012-9918-x
- Bengtson, Bradley P. "Complications, reoperations, and revisions in breast augmentation." Clinics in plastic surgery 36.1 (2009): 139-156.
- Sá dos Reis, Cláudia, Isabelle Gremion, and Nicole Richli Meystre. "Study of breast implants mammography examinations for identification of suitable image quality criteria." Insights into imaging 11 (2020): 1-11.
- Spear, Scott L., and James L. Baker Jr. "Classification of capsular contracture after prosthetic breast reconstruction." Plastic and reconstructive surgery 96.5 (1995): 1119-1123.
- di Pompeo, Fabio Santanelli, and Michail Sorotos. "EURAPS editorial: BIA-ALCL, a brief overview." Journal of Plastic, Reconstructive & Aesthetic Surgery 71.6 (2018): 785-787.
- Serena TJ, Habib P, Derosa A. Breast Implant Illness: A Cohort Study. Cureus. 2023 Apr 24;15(4):e38056. doi: 10.7759/cureus.38056. PMID: 37228535; PMCID: PMC10208020.


