Summary Card
Definition
Gynaecomastia is enlargement of the male breast, caused by glandular proliferation and fat deposition.
Pathophysiology
An imbalance of androgenic and oestrogenic effects on the breast.
Clinical Features
Bilateral, firm, concentric, and painless enlargement of the male breast.
Classification
Simon's classification is based on the degree of tissue and skin excess and Cordova is based on structural components of the breast. Gynaecomastia is staged using the Rohrich et al staging system.
Investigations
Detailed medical history, clinical examination, specific blood tests, ± imaging ± tissue sampling.
Treatment
Weight loss, reassurance, pharmacotherapy, and surgical resection or liposuction.
Complications
Complications of surgical excision include NAC loss, deformity, over/under resection, scarring, and recurrence.
Primary Contributor: Dr Waruguru Wanjau, Educational Fellow.
Reviewer: Dr Suzanne Thomson, Educational Fellow.
Definition of Gynaecomastia
Gynaecomastia (GM) is characterised by enlargement of the male breast, caused by glandular proliferation and fat deposition.
Gynaecomastia is defined as generalised enlargement of male breast tissue, with the presence of a rubbery or firm mass extending concentrically and symmetrically from the nipple. Histologically, it involves a benign proliferation of glandular tissue in the male breast (Cuhaci, 2014).
Pseudogynaecomastia is common in obese men, and consists of lipomastia alone, without glandular proliferation.
Pathophysiology of Gynaecomastia
Gynaecomastia arises from an imbalance between androgenic and oestrogenic effects on breast tissue.
Gynaecomastia results from an imbalance in breast tissue, where oestrogenic effects outweigh androgenic effects. Causes include:
- Elevated estradiol levels.
- Increased local oestrogen production.
- Excess testosterone.
- Increased aromatase activity converting androgens to oestrogens.
Increased Oestrogen
Increased oestrogen levels contribute significantly to gynaecomastia. This can result from:
- Production: High levels of free oestrogens secreted by testes or adrenal glands
- Metabolism: Extraglandular aromatization of oestrogen precursors, reduced degradation of oestrogens.
- Exposure: Oestrogen-like chemicals, exogenous oestrogens, or drugs displacing oestrogen more than androgen from SHBG.
Decreased Testosterone
Decreased testosterone levels contribute to gynaecomastia. This can result from:
- Production: Decreased androgen production in the testes
- Metabolism: Altered androgen metabolism, Increased binding of androgens (relative to oestrogens) by SHBG
- Exposure: Drug-induced displacement of androgens from their receptors and androgen receptor defects
Aetiology of Gynaecomastia
Gynaecomastia can be idiopathic, physiological (trimodal distribution) or pathological.
The aetiology of gynaecomastia can be categorised into three main areas: idiopathic, physiological, and pathological.
Physiological
Physiological gynaecomastia has the classic trimodal distribution. The 3 time periods commonly affected are
- Newborns: 60-90% affected by maternal oestrogen transfer; resolves within the first year.
- Puberty: Up to 65% affected by temporary oestrogen elevation; 90% resolve spontaneously.
- Elderly: declining testosterone levels, medications, & other factors.
These 3 periods are explained in greater detail in the image below.
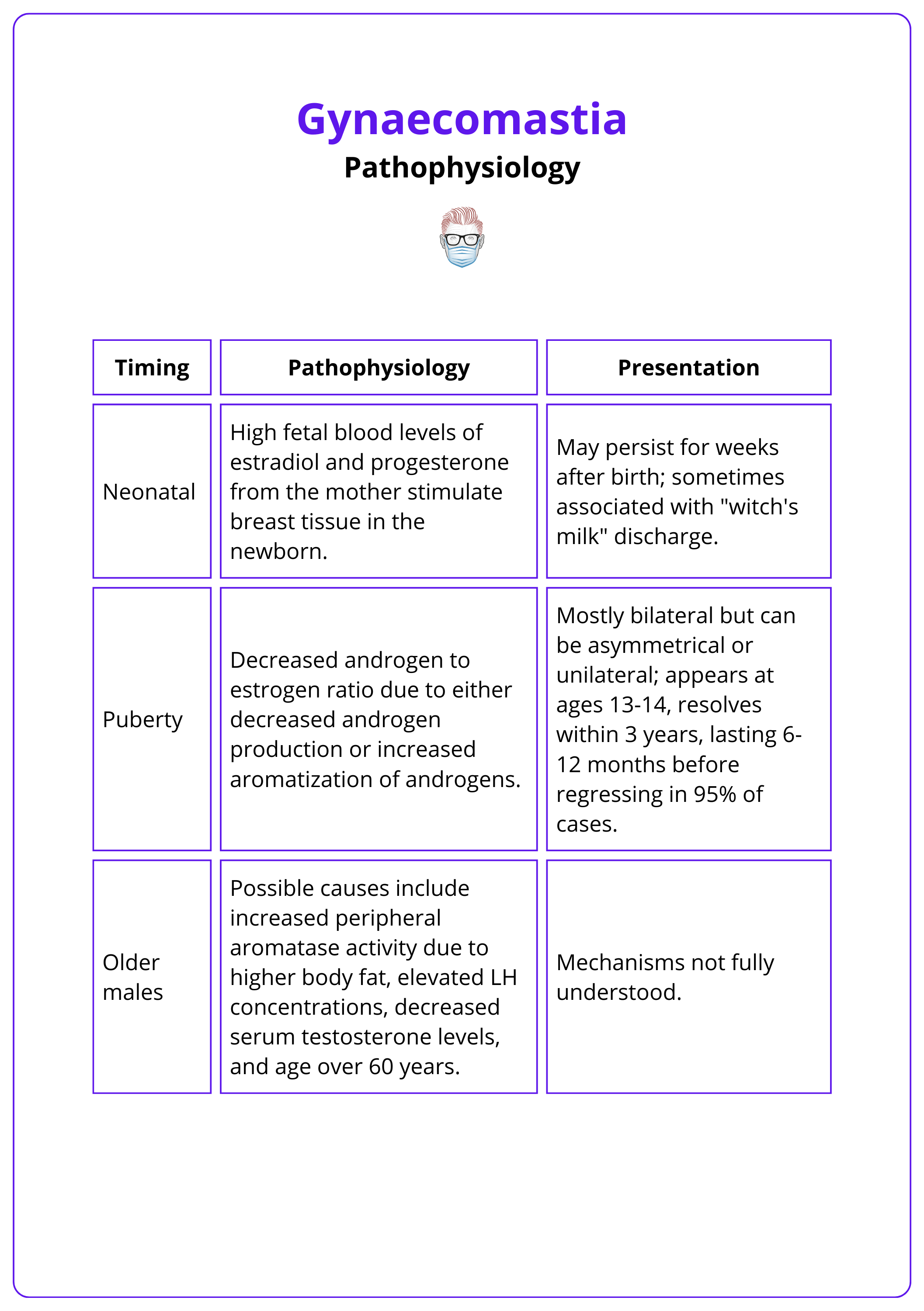
Pathological
Pathological causes are less common, but thorough investigations should still be considered. In the clinical history, red flags:
- Medications (Barros, 2012): Anti-androgens, Steroids, Psychiatric medications, Anti-hypertensives.
- Drugs: Amphetamines, alcohol and marijuana
The below table details other pathological causes of gynaecomastia.
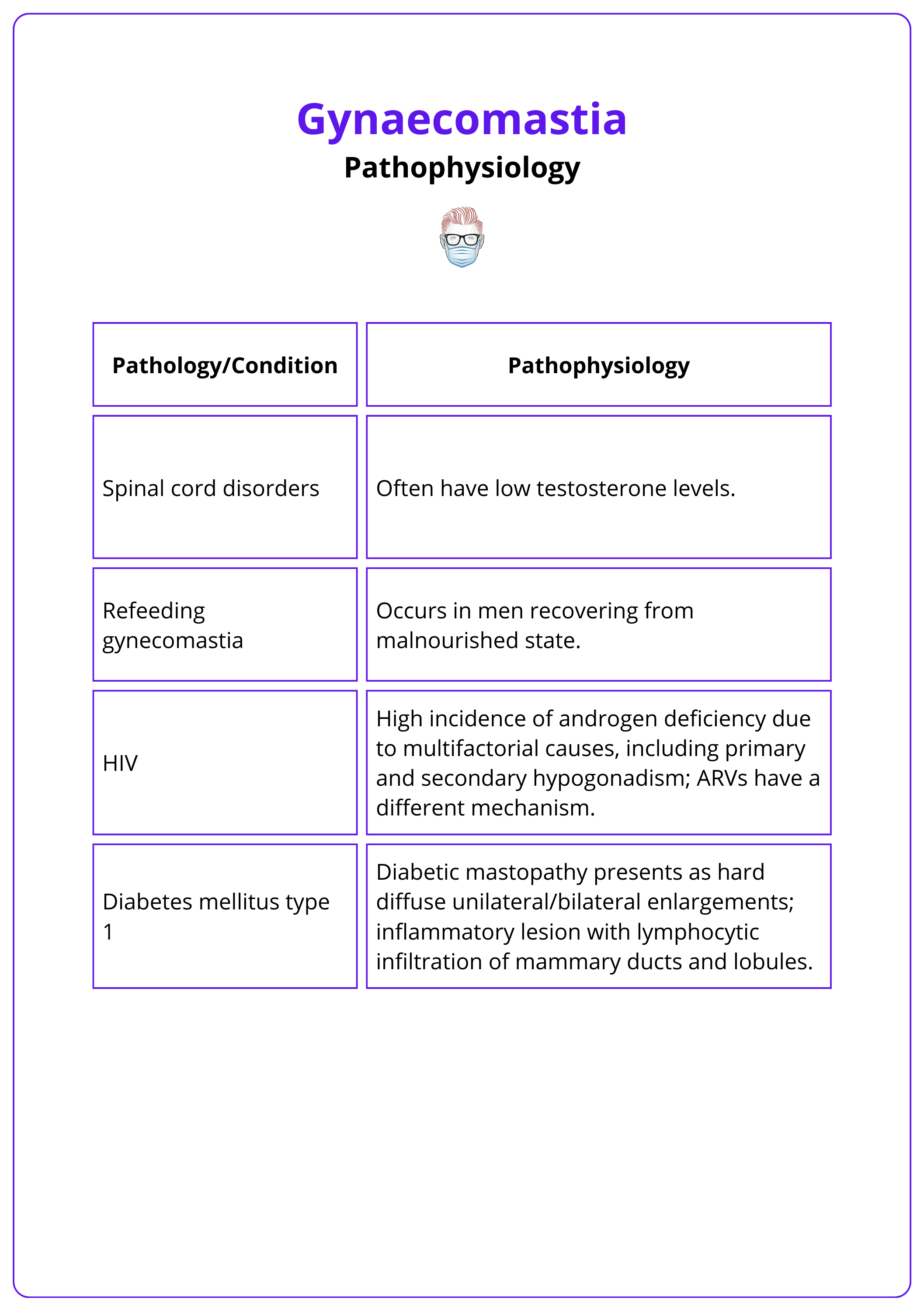
Spironolactone causes gynaecomastia by several mechanisms, it blocks testosterone synthesis, blocks androgen action, and displaces oestrogen from SHBG (Swerdloff, 2023).
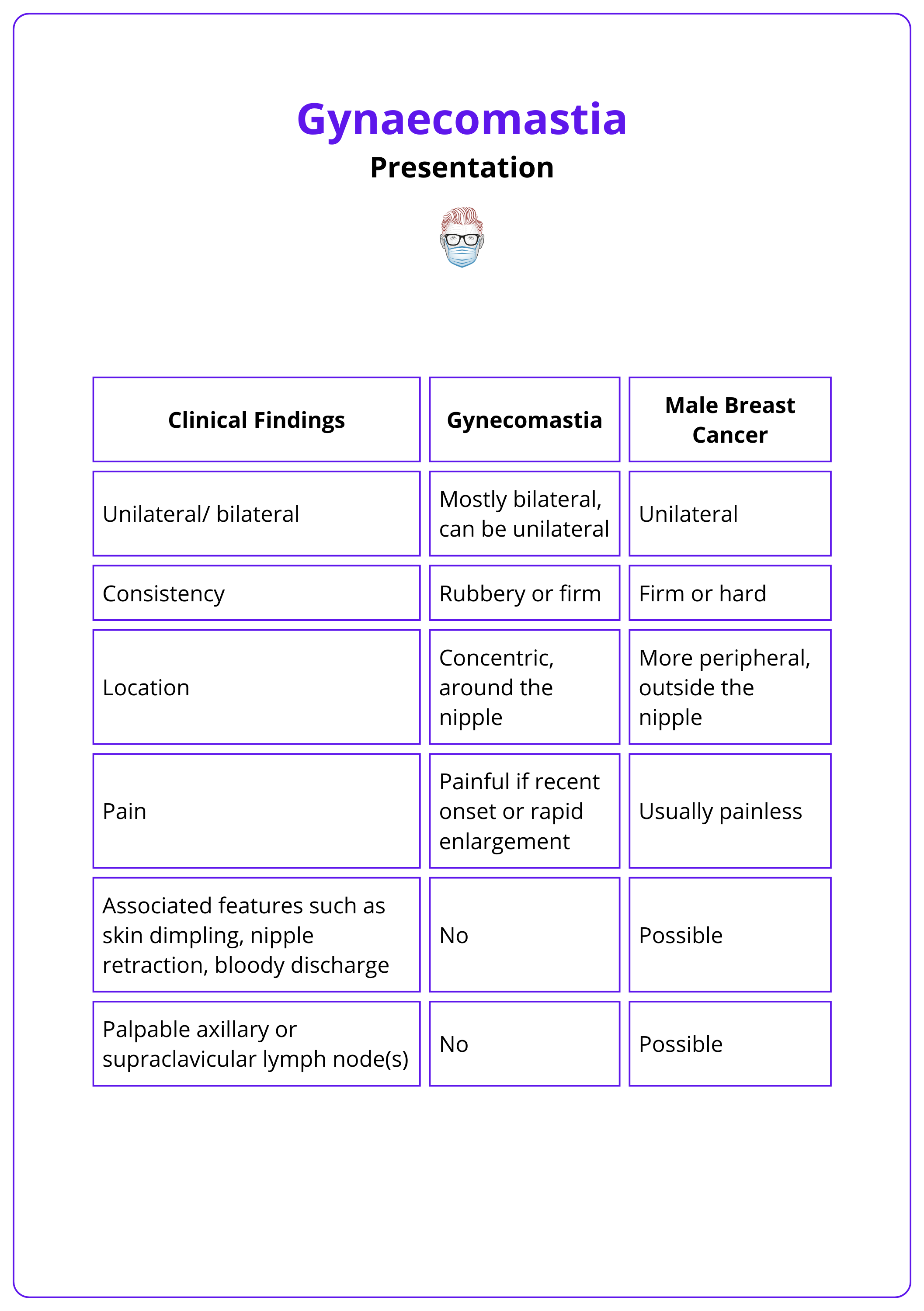
Clinical Features of Gynaecomastia
Gynaecomastia presents as bilateral, firm, concentric, painless enlargement of the male breast
The classic clinical feature of gynaecomastia is bilateral, firm, concentric breast enlargement in the absence of skin changes. It is important to differentiate true gynaecomastia from pseudo-gynaecomastia, and male breast cancer.
Key points to consider in the history include:
- Patient Status: Age, Medications, Drugs (Anabolic, Recreational)
- Symptoms: Duration, tenderness/pain, weight changes
- Systemic: liver disease, malnutrition, kidney failure, thyroid, adrenal disease.
It is important to document the following on examination:
- Inspection: ptosis, skin excess
- Palpation: masses
- Specific: fat versus glandular predominance via Pinch test
- Other areas: genitals, thyroid, GI examination (liver disease)
Key physical features of gynecomastia are detailed in the table below, adapted from Swerdloff, 2023.
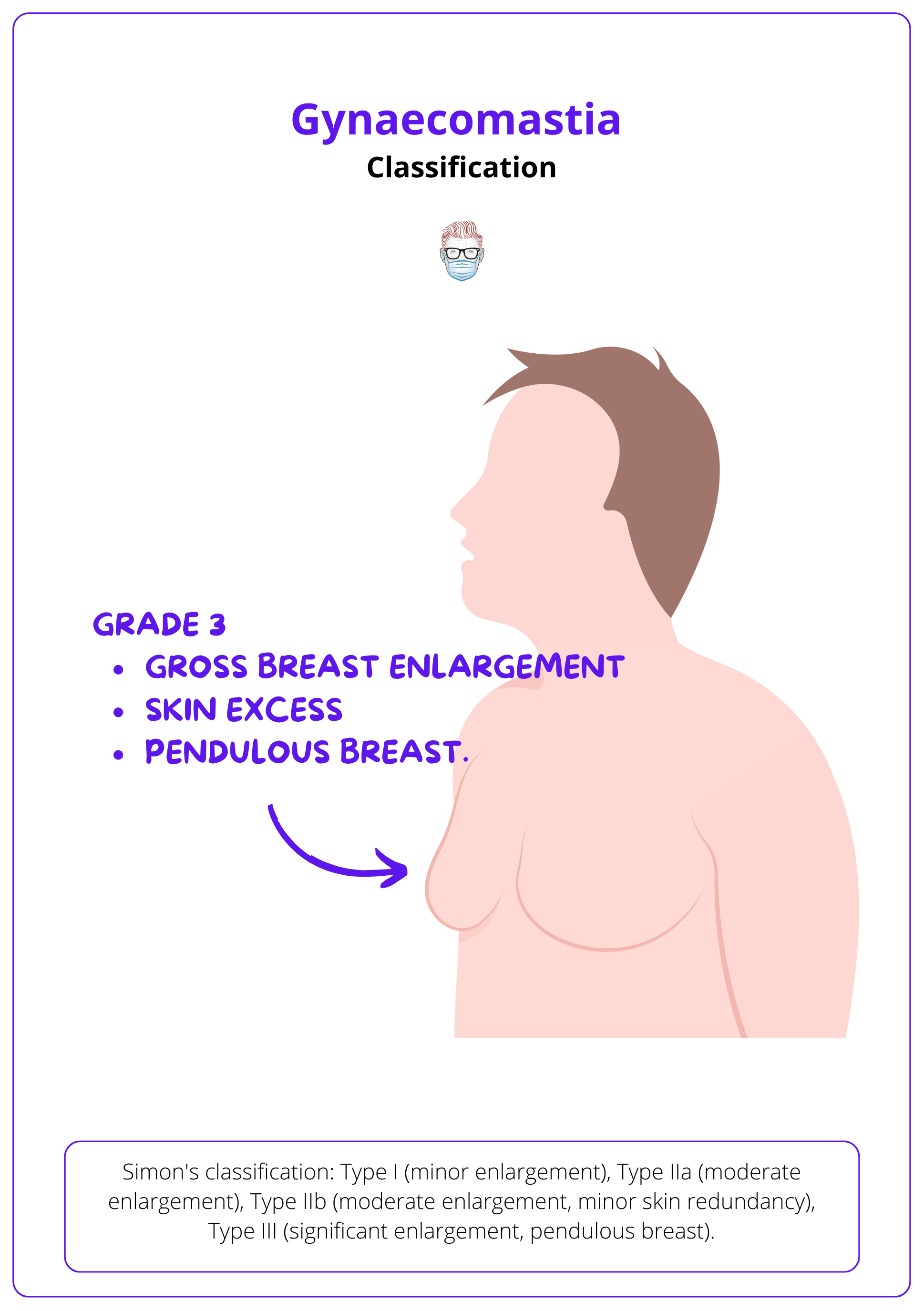
Classification of Gynaecomastia
Simons grade is based on the degree of tissue and skin excess. Cordova considers structural components of the breast. Rohrich stages are based on the degree of hypertrophy and fibrosis.
The staging and presentation of gynecomastia are crucial in determining the appropriate management options. The most commonly used classification system for this purpose is the Simon Classification, detailed below.
Simon Classification
Simon classification is based on the degree of tissue and skin excess.
- Type I: minor breast enlargement without skin excess.
- Type IIa: moderate breast enlargement without skin excess.
- Type IIb: moderate breast enlargement with minor skin redundancy.
- Type III: gross breast enlargement with skin excess creating a pendulous breast.
This classification can be visualised in the image below.
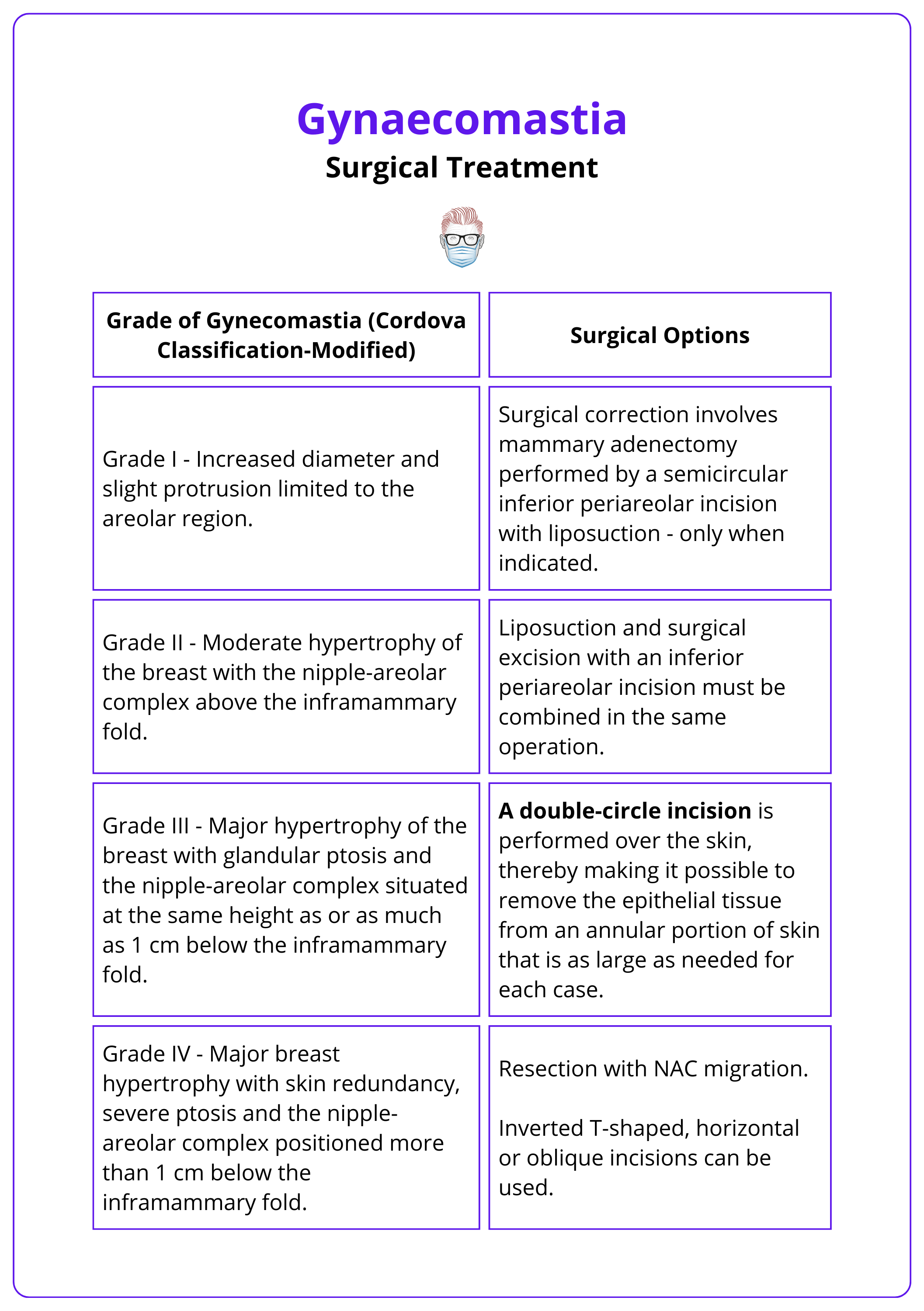
Cordova Classification
Cordova and Moschella classification takes into account the different structural components of the breast, the relationship with the IMF, and the NAC.
- Grade I: increase in diameter and protrusion limited to the areola.
- Grade II: hypertrophy of all the components of the breast; NAC is above the IMF.
- Grade III: hypertrophy of all the components; NAC at the same height as or 1 cm below the IMF.
- Grade IV: hypertrophy of all the components; NAC >1cm below the IMF.
Rohrich Staging
The Rohrich Classification system is used to stage gynecomastia based on the degree of hypertrophy and ptosis:
- Grade I: Minimal hypertrophy (<250g) with no ptosis
- Ia - primarily glandular
- Ib - primarily fibrous
- Grade II: Moderate hypertrophy (250-500g) with no ptosis
- IIa - primarily glandular
- IIb - primarily fibrous
- Grade III: Severe hypertrophy (>500g) with grade I ptosis
- Grade IV: Severe hypertrophy with grade II or III ptosis
Gynecomastia does not increase the risk of male breast cancer. However, patients with Klinefelter syndrome have up to 50 times higher risk of developing breast cancer.
Investigations for Gynaecomastia
Routine evaluation of gynaecomastia includes specific blood tests, imaging, and tissue sampling, often involving an endocrinologist.
Laboratory
Routine laboratory investigations focus on identifying any treatable endocrinological cause.
- Bloods: Liver Profile, Testosterone, TSH/free thyroxine, LH, hCG, prolactin
- If small, firm testes: Karyotyping for 47XXY
- If abnormal testicular mass: ultrasound, beta-hCG, FSH, LH, serum testosterone, or oestradiol
Imaging
Imaging is not routinely performed in the pre-operative workup of gynecomastia. Typical breast ultrasound findings include hypoechoic retroareolar masses and increased anteroposterior depth at the nipple. Imaging considerations include:
- Mammography: If malignancy is suspected ± histology
- Ultrasound: Adrenal glands and testes, if indicated. ± histology
Treatment of Gynaecomastia
Treatment options include weight loss, reassurance, medical pharmacotherapy, and surgical correction.
Treatment for gynaecomastia varies based on aetiology and severity. Before any intervention, it is essential to stop causative medications or treat underlying endocrine or systemic conditions.
Mild cases typically focus on reassurance, diet, and exercise, while more severe cases may require medical or surgical treatment. This is explained in more detail below.
Most cases of pubertal gynecomastia resolve spontaneously within one to two years, but about 20% of patients have residual gynecomastia by age 20.
Medical Treatment
Medical treatment for gynecomastia is considered in cases that are severe, persistent, or of recent onset (less than 6 months). If there is no treatable underlying cause, 3 classes of medical therapies can be considered
- Androgens: testosterone, dihydrotestosterone, danazol.
- Anti-oestrogens: clomiphene citrate, tamoxifen (up to 80% of patients report complete resolution, Bedognetti, 2009).
- Aromatase inhibitors: letrozole, anastrozole (Braunstein, 2007).
Prophylactic breast irradiation can reduce gynecomastia in patients on long-term antiandrogen therapy (e.g., prostate cancer), but it carries a theoretical risk of tumorigenesis and is not indicated for idiopathic gynecomastia.
Medical treatment is most effective when started before the glandular structure is replaced by stromal hyalinization and fibrosis.
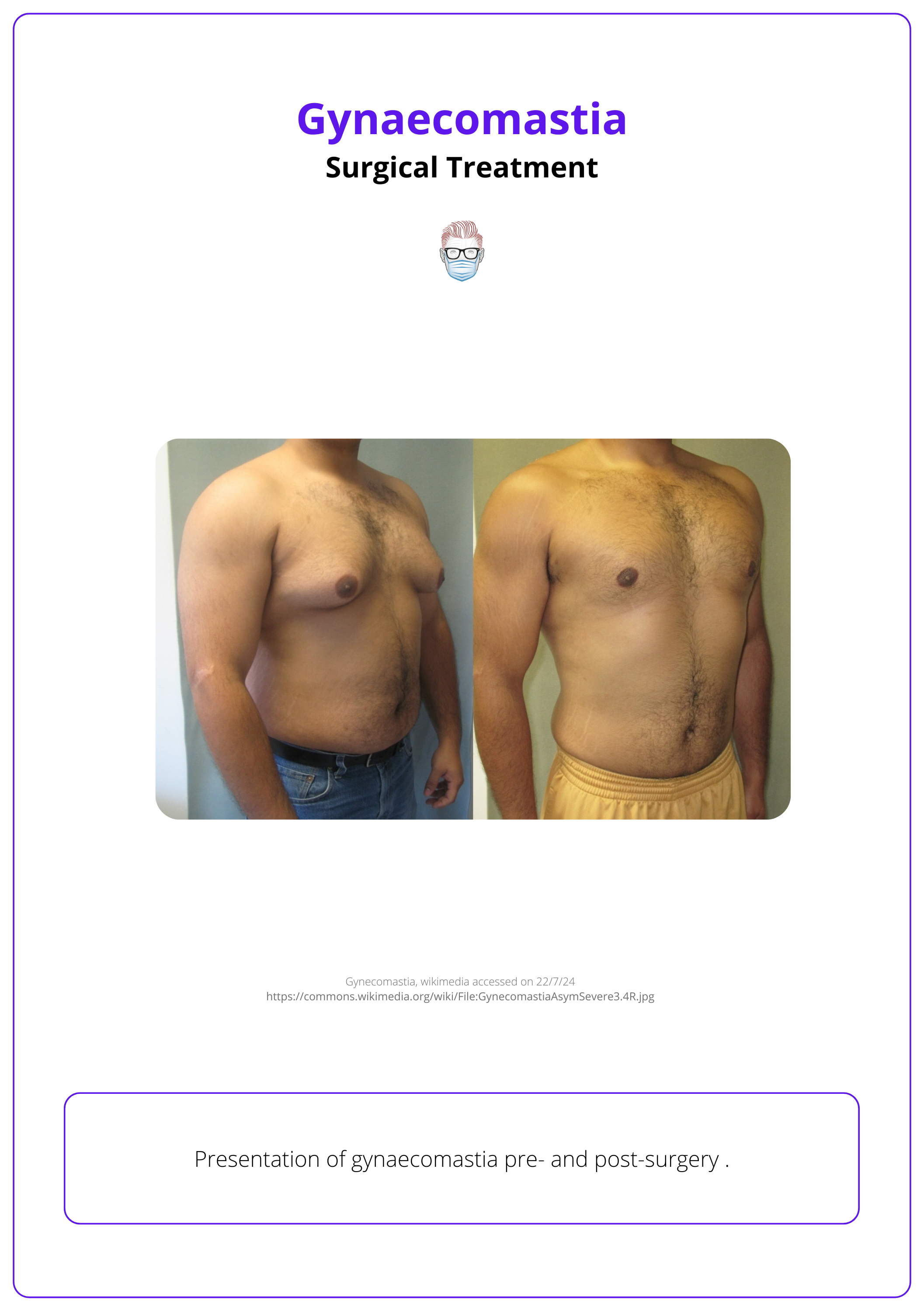
Surgical Treatment for Gynaecomastia
Surgery is useful in the management of patients with long-standing symptomatic gynaecomastia or when medical therapy is not successful.
Indications for Surgery
Surgery aims to reduce the size of the breast with minimal scars possible. It is indicated in:
- Symptomatic patients
- Breast changes: fibrosis, risk for carcinoma (e.g. Klinefelter's syndrome)
- Medical Therapy has been ineffective
- Interferes with the patient's activities of daily living
Types of Surgery
The decision-making process for gynaecomastia should focus on: technique (liposuction vs resection vs combination), single vs two-stage, and timing.
In relation to liposuction, options include:
- Manual liposuction
- Power-assisted liposuction: Reduces operative fatigue and improves control in chest wall contouring
- Ultrasound-assisted liposuction (UAL): Associated with improved skin retraction
- Laser-assisted liposuction
In relation to surgical excision, design options include:
- Nipple Incisions: Periareolar, Circumareolar
- Breast Incisions: Wise pattern, IMF +/- free nipple graft
In relation to timing of surgery, considerations include:
- Delayed until the underlying cause of gynaecomastia has been treated.
- Delayed in pubertal gynaecomastia til after completion of puberty when possible, to minimize the chance of recurrent gynaecomastia after surgery.
Surgical approaches for gynaecomastia are detailed in the table below – adapted from (Baros, 2012).
Two-stage surgery is indicated for significant excess skin and grade III Renault ptosis over hypertrophied pectoralis muscles, commonly seen in bodybuilders after steroid use.
Complications of Gynaecomastia
Complications of surgical excision include NAC loss, deformity, over/under resection, scarring, and recurrence.
Surgical excision for gynaecomastia can lead to several complications, including NAC (nipple-areolar complex) loss, deformity, over- or under-resection, scarring, and recurrence.
- Over-resection: Over-correction can result in a sunken nipple, known as "saucer deformity," where the nipple adheres to the underlying muscle due to the lack of subcutaneous tissue.
- Scarring: Noticeable scars may form, affecting the cosmetic outcome.
- Recurrence: Gynecomastia can recur if the underlying cause is not addressed.
- Nipple-Areolar Complex: Loss or compromise of the NAC can lead to significant deformity.
- Early Postoperative Complications: These can include haematoma, seroma, infection, and wound healing problems, often related to the anaesthesia and surgical process.
Effective surgical planning and careful postoperative care are essential to minimize these risks and achieve the best results for patients undergoing gynecomastia surgery.
Conclusion
1. Understanding of Gynaecomastia: This includes knowledge about its definition, pathophysiology, classification, and how it presents clinically.
2. Diagnostic Process: Recognized the importance of a detailed medical history, clinical examination, specific blood tests, imaging, and potentially tissue sampling for the effective diagnosis of gynaecomastia.
3. Treatment Options: Understood various treatment strategies from conservative approaches like reassurance and weight loss to pharmacological treatments and surgical interventions.
4. Surgical Techniques and Complications: Familiarized with different surgical approaches for the management of gynaecomastia and learned about potential complications associated with these surgeries.
Further Reading
- Swerdloff RS, Ng JCM. Gynecomastia: Etiology, Diagnosis, and Treatment. [Updated 2023 Jan 6]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279105/
- Cuhaci N, Polat SB, Evranos B, Ersoy R, Cakir B. Gynecomastia: Clinical evaluation and management. Indian J Endocrinol Metab. 2014 Mar;18(2):150-8. doi: 10.4103/2230-8210.129104. PMID: 24741509; PMCID: PMC3987263.
- Ali SN, Jayasena CN, Sam AH. Which patients with gynaecomastia require more detailed investigation? Clin Endocrinol (Oxf). 2018 Mar;88(3):360-363. doi: 10.1111/cen.13526. Epub 2017 Dec 21. PMID: 29193251.
- Narula HS, Carlson HE. Gynecomastia. Endocrinol Metab Clin North Am. 2007 Jun;36(2):497-519. doi: 10.1016/j.ecl.2007.03.013. PMID: 17543732.
- Barros AC, Sampaio Mde C. Gynecomastia: physiopathology, evaluation and treatment. Sao Paulo Med J. 2012;130(3):187-97. doi: 10.1590/s1516-31802012000300009. PMID: 22790552; PMCID: PMC10876201.
- Braunstein GD. Clinical practice. Gynecomastia. N Engl J Med. 2007 Sep 20;357(12):1229-37. doi: 10.1056/NEJMcp070677. PMID: 17881754.
- Bedognetti D, Rubagotti A, Conti G, Francesca F, De Cobelli O, Canclini L, Gallucci M, Aragona F, Di Tonno P, Cortellini P, Martorana G, Lapini A, Boccardo F. An open, randomised, multicentre, phase 3 trial comparing the efficacy of two tamoxifen schedules in preventing gynaecomastia induced by bicalutamide monotherapy in prostate cancer patients. Eur Urol. 2010 Feb;57(2):238-45. doi: 10.1016/j.eururo.2009.05.019. Epub 2009 May 19. PMID: 19481335.
- Godwin Y. Correction of Tuberous Nipple Areolar Complex Deformity in Gynecomastia: The Deformity That Can Get Forgotten. Ann Plast Surg. 2018 Jul;81(1):3-6. doi: 10.1097/SAP.0000000000001442. PMID: 29762454.


